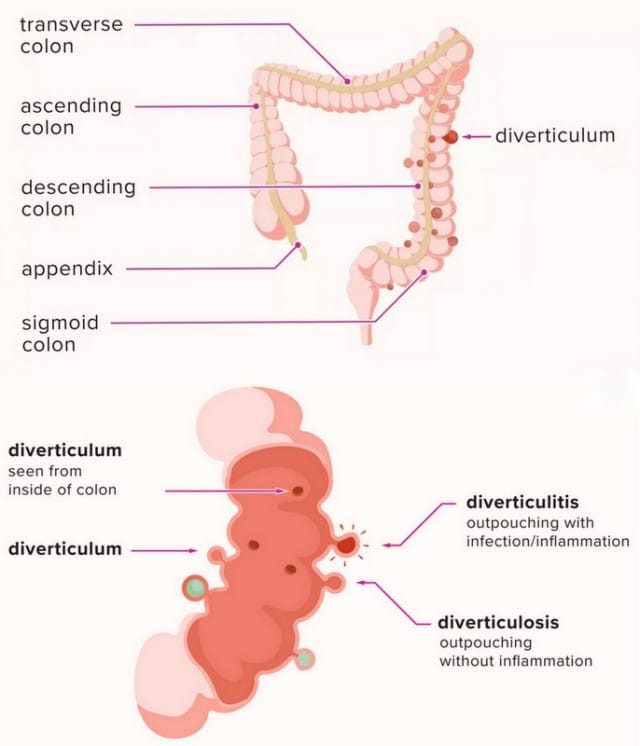
Diverticulosis is the process in which small bulges or pockets (diverticula) form in the in the wall of the large intestine or colon (Queensland Health, 2019). Diverticula generally form when naturally weak areas of the lower gastrointestinal tract give way under pressure, causing small pockets (about the size of a marble) to protrude through the wall. For most people, these pockets won’t cause any symptoms or problems. If the diverticulum becomes infected or inflamed, it becomes known as diverticulitis and can be uncomfortable and pose health risks to the individual (Queensland Health, 2019). Diverticulitis is linked to a low-fibre diet and is increasingly common with age. 1 in 3 Australians aged 45 have diverticular disease, and 2 in 3 Australians aged over 85 (Health Direct, 2020) (Digestive Health Foundation, 2009).
Symptoms
The most common symptom in people with diverticulitis is pain, which can be mild or severe, usually felt on the left lower side of the abdomen. Other symptoms include:
- Abdominal pain or tenderness
- Fever
- Nausea and vomiting
- Constipation or (less commonly) diarrhoea
- Feeling bloated
- Blood in the stool from diverticular bleeding
- Mucus in the stool
These symptoms may be mild or severe, depending on the extent of the infection and any complications. You should see your doctor immediately if you have any of the following symptoms:
- Very severe abdominal pain
- A fever
- Feel very unwell
- Blood in stool
Risk Factors
- Age: the incidence of diverticulitis increases with age
- Obesity: increased BMI increases likeliness of developing this condition
- Smoking: smoking increases likeliness of developing this condition
- Lack of exercise: regular exercise appears to lower your risk of diverticulitis
- Diet: diets high in animal fat and low in fibre tend to have an increased risk of developing this condition. Less fibre increases constipation, and results in harder stool that are more difficult to push along the colon. The increased pressure required to move the stool may lead to ‘blow outs’ in the colon and form what we can diverticular or pockets.
Diagnosis
Your GP will take a history and examine you. If diverticulitis is suspected, your GP may request a colonoscopy, a barium enema or an abdominal CT scan to confirm.
Treatment
Treatment is focused on clearing the infection and inflammation, pain relief, colon rest and prevention or minimising of complications. For mild conditions, you may be treated at home with a low fibre diet or liquid diet to rest the bowel. Antibiotics may be prescribed to clear the infection and mild pain relief such as paracetamol. For more severe diverticulitis, patients may require hospital admission with antibiotics and fluids given directly into the vein through a ‘drip’. In few cases, complications may develop such as bowel perforation, abscess or uncontrollable bleeding. In this case, surgery may be required to remove the diseased segment of colon.
Prevention
To help prevent diverticula from developing, we recommend a diet high in fibre including lots of fruits, vegetables, legumes, and wholegrains. We also suggest increasing water intake to at least 8 cups of water per day, and regular exercise. For advice or assistance in incorporating these preventative strategies in your life, book in to see our GP or dietitians.
The information in this article has been adapted from:
Digestive Health Foundation. (2009). Diverticular Disease. Retrieved from Gastroenteroligical Society of Australia: https://www.gesa.org.au/resources/patients/diverticular-disease/#:~:text=Only%20about%20a%20quarter%20of,used%20to%20diagnose%20diverticular%20disease.
Health Direct. (2020). Divertiucular disease – diverticulitis and diverticulosis. Retrieved from Health Direct : https://www.healthdirect.gov.au/diverticular-disease-and-diverticulitis
Queensland Health. (2019). The common condition you may never have heard of: what is diverticulitis and how do you prevent it? Retrieved from Queensland Government: Queensland Health: https://www.health.qld.gov.au/news-events/news/diverticulitis
This article was written by April Stevens BSc. MD student.
27th October 2020.


